Dry eye disease is a serious issue during the menopause transition and may have a significant impact on quality of life. A recent review in the Journal of Mid-life Health has drawn attention to the high prevalence of dry eye disease in the perimenopause and the role hormones play in this condition.(1)
Dry eye disease (also known as DED) affects the surface of the eye and may cause eye pain, inflammation, general discomfort and may also impact eyesight and cause visual disturbance. Around 7% of women over 50 years are thought to suffer with DED.
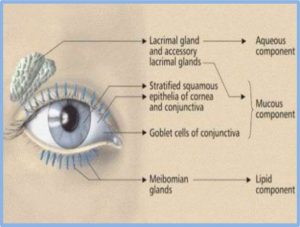
Research has found that hormone levels have a direct effect on eye health. In particular hormones influence the complex components of the tear film that covers and protects the eye. Multiple glands and specialised cells are involved in producing the tear film (Figure 1) and there are many factors such as drainage, evaporation rate, tear production and the health of the glands and the immune system that may influence DED.
Figure 1. The aqueous, mucous and lipid components of the tear film.
It is known the hormones such as estrogen and testosterone play an important role in eye health and are likely to be culprits in the increased risk of DED in perimenopausal women.
The authors of the review, Dr Travis Peck, MD, and colleagues at the Department of Ophthalmology, University of Virginia, USA, explain that:
“Both androgens and estrogen have known effects on the synthesis and components of the tear film. Sex steroid receptors are present on the meibomian glands, which are the sebaceous glands on the eyelids responsible for producing the oil component of tears that prevents evaporation.”(1)
Interestingly, scientific studies have reported that women on long-term hormone replacement therapy (HRT) report fewer eye health issues. (2,3) It has also been established that men and women on testosterone therapy have a decreased risk of DED.
New developments in delivering androgens directly to the eye via eye drops or using a spray to the tissue surrounding the eye are showing promising results, however there is a need for larger clinical trials to provide further evidence.
Dr Peck concluded that:
“Given high prevalence of DED, it is important for gynecologists and for primary care physicians to understand DED to recognize symptoms and start initial lubricating therapy and identify patients who would benefit from ophthalmology referral for further interventions.”(1)
The full review article can be accessed here.
I invite you to (anonymously) participate in ‘The Perimenopause Project’ by sharing your personal experience of the perimenopause for the benefit of other women.
Please read my disclaimer here and always consult your physician for health related advice.
References
1) Peck T, Olsakovsky L, Aggarwal S. Dry Eye Syndrome in Menopause and Perimenopausal Age Group. J Midlife Health. 2017 Apr-Jun;8(2):51-54. doi: 10.4103/jmh.JMH_41_17.
2) Jensen AA, Higginbotham EJ, Guzinski GM, Davis IL, Ellish NJ. A survey of ocular complaints in postmenopausal women. J Assoc Acad Minor Phys 2000;11:44‑9.
3) Sullivan DA, Sullivan BD, Evans JE, Schirra F, Yamagami H,Liu M, et al. Androgen deficiency, Meibomian gland dysfunction, and evaporative dry eye. Ann N Y Acad Sci 2002;966:211‑22.